There are different scoliosis treatment approaches for patients, and their families, to choose between. The two main treatment approaches are traditional and conservative: the former funnels patients towards spinal fusion surgery, while the latter works towards achieving a curvature reduction through proactive treatment.
Spinal fusion surgery has the goal of preventing progression and is part of the traditional scoliosis treatment approach; however, there are other treatment options available, and spinal fusion is lengthy, invasive, and carries some heavy potential side effects and risk of complications.
Let’s start our discussion of scoliosis treatment options with the traditional approach, as it has been the dominant approach for many years and continues to funnel patients towards spinal fusion surgery.
The Traditional Scoliosis Treatment Approach
As mentioned, there are two main scoliosis treatment approaches: traditional and conservative.
The traditional approach has been in place for hundreds of years, and the general path of treatment includes diagnosis, watching and waiting, traditional bracing, and surgical recommendations.
The condition’s most common type is adolescent idiopathic scoliosis (AIS), diagnosed between the age of 10 and 18, so our focus is on surgery for treating scoliosis in adolescents.
Now, this age group is entering into, or is in, the stage of puberty, characterized by rapid and unpredictable growth spurts, and while we don’t know what causes idiopathic scoliosis, we know what triggers its progressive nature: growth and development.
Important condition characteristics to understand is that it’s progressive, meaning it will get worse over time, particularly if left untreated, or not treated proactively, and that scoliosis develops across a wide severity spectrum of mild to moderate and severe to very severe.
For an adolescent recently diagnosed with mild scoliosis on the traditional path of treatment, they are likely going to be told that as their condition is mild, they should return for periodic examinations to monitor for further progression: meaning the unnatural sideways spinal curve, with rotation, is increasing in size.
The danger with this is that as growth is the main progressive trigger, what if this patient has a huge growth spurt in between doctor’s visits and progresses into the moderate stage; basically, that curvature has been allowed to progress unimpeded, rather than making efforts to reduce the curve while mild, while it’s at its most flexible, prior to progression and the body having had time to adjust to its presence, and when the spine is going to be most responsive to treatment.
Now what’s likely to happen is continued monitoring, until the patient progresses well into the moderate stage when traditional scoliosis bracing is the only actual form of treatment applied, but traditional bracing has a lot of shortfalls that limit its efficacy.
If bracing has proved ineffective at stopping progression, once a condition passes that surgical level threshold at 40+ degrees and shows signs of continued progression, in many cases, that patient would be given a spinal fusion surgical recommendation.
A question to keep in mind is what might have happened had proactive treatment been applied as soon as the young patient received their diagnosis, rather than the focus being on watching and waiting?
What is Spinal Fusion Surgery?
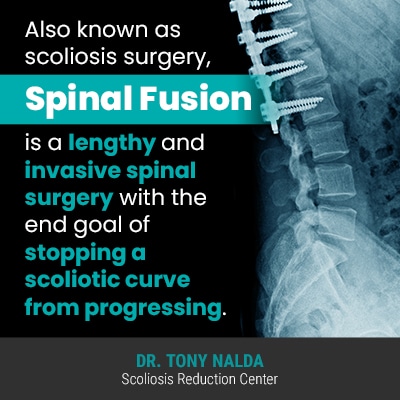
Also known as scoliosis surgery, spinal fusion is a lengthy and invasive spinal surgery with the end goal of stopping a scoliotic curve from progressing.
Spinal fusion surgery involves the fusing together of multiple vertebrae (bones of the spine) into one solid bone; this involves the most-tilted vertebrae at the apex of the unnatural spinal curve.
In addition, hardware is attached to the spine, most often in the form of rods and screws, to hold the spine in place while the fusion continues to heal.
The hardware will be attached to the spine forever, and if the hardware should fail, or there is an adverse reaction to the foreign elements inside the body, there is no recourse other than subsequent surgeries.
The idea is that as the most-tilted vertebrae become fused into one solid bone, it eliminates movement in the area (progression), but what this also equates to is a loss of spinal mobility in the area: an outcome many patients are disappointed with.
The surgery also comes with other risks patients, and their families, should be aware of, and of course, although stopping progression is the surgical goal, there are no guarantees.
Spinal Fusion Surgery Risks
While spinal surgeons have their patients’ best interests at heart, any surgical procedure comes with its share of risks, and spinal fusion is no exception.
When weighing out the pros and cons of spinal fusion, patients should fully understand all the potential risks and side effects, not to mention knowing what it can be like to live with a fused spine.
Following are some potential risks associated with the surgery itself:
- Risk of infection
- Excessive blood loss
- Nerve damage
- Fusion-site pain
- Need for subsequent surgeries
In addition to the aforementioned risks associated with the surgical procedure itself, there are numerous side effects to living with a fused spine, and these are what I want patients to really be aware of, because there are different potential treatment outcomes patients can choose between.
What I find the most disheartening is when patients come to me post-surgery and are disappointed with the results, but had no knowledge that there were other treatment options available.
While scoliosis surgery has its place in treatment, as it is such an invasive and permanent option, I feel patients should explore less-invasive options first.
Following are some potential post-surgical side effects patients need to be aware of:
- Significant loss of spinal mobility/flexibility
- Neurological damage
- Pain
- Adverse reaction to hardware
- Hardware failure/deterioration over time
- Continued curvature progression
- Psychological effects of living with a fused spine
Like any spinal surgery and/or condition, every case is different, but what many patients express to me post spinal fusion is that the loss of spinal flexibility has cost them a certain quality of life: once-loved activities can become more difficult, and the fear of trying new things with a fused spine can be a very-real psychological side effect.
Loss of spinal mobility/flexibility will depend on many factors such as patient age and overall health, condition severity, fusion location, and the amount of vertebrae involved.
Unfortunately, a spine that is more rigid is a spine that’s more likely to cause pain, and increasing pain is a common reason for requiring subsequent surgeries.
The main reason many patients, particularly adolescents, opt for spinal fusion is for cosmetic reasons: they want a full return to their pre-scoliosis bodies and think that surgery is the best chance of that.
Sadly, spinal fusion is rarely able to fully correct the related postural deviation that scoliosis causes, and this is another factor many patients are disappointed with and don’t fully expect.
There is also the recovery process/time to think about, and for some, this can be lengthy.
How Painful is Spinal Fusion Recovery?
Each patient will recover at their own pace, and spinal fusion recovery time and pain levels will depend on many factors: patient age and overall health, curvature location, condition severity, number of vertebrae fused, whether or not there were complications during the surgery, etc.
For most, recovery will take place at home with activity restrictions such as no bending, lifting, or twisting, and performing these movements too early will be painful.
Patients will be heavily medicated for the days immediately following the surgery, with the goal of weaning the patient off meds as soon as possible.
Most patients are completely off pain medication within 6 weeks of surgery, but again, each case is unique, with some remaining on medication beyond that, and some coming off earlier.
Most patients will receive their first check up within 2 weeks following the surgery, and activity restrictions and pain meds will be adjusted accordingly, with many patients being cleared for regular activity within 4 to 6 weeks post-surgery, barring any complications.
Remember, there are also nonsurgical scoliosis treatment options available for patients to try first, and when successful, these come with numerous benefits.
The Conservative Treatment Approach and Nonsurgical Treatment Options
Here at the Scoliosis Reduction Center®, I offer patients a conservative scoliosis treatment approach that prioritizes the spine’s overall health and function throughout treatment and beyond.
While there are never treatment guarantees, for those who choose to forego a surgical recommendation, with hard work and commitment, I can help patients reduce surgical-level curves and avoid the need for invasive and costly surgery.
I integrate multiple forms of treatment so each and every treatment plan can be fully customized to address important patient/condition variables.
I believe in starting proactive treatment as close to the time of diagnosis as possible because, as a progressive condition, where a patient’s scoliosis is at the time of diagnosis is not indicative of where it will stay.
If I see a patient diagnosed with mild scoliosis, I see it as an opportunity to keep it that way: to prevent further progression, increasing condition severity, escalating symptoms, and the need for more invasive treatment in the future.
By combining condition-specific chiropractic care, in-office therapy, custom-prescribed home exercises, and corrective bracing, I can help patients work towards achieving a curvature reduction on a structural level, increasing core strength so the spine is optimally supported and stabilized, and corrective bracing can help augment corrective treatment results.
The end goal of conservative treatment is not solely to prevent progression, but rather to actually correct the scoliosis by restoring as much of the spine’s healthy curves as possible and preserving the spine’s overall function.
Conclusion
The best advice I can give to patients recently diagnosed, and their families, is to do their own due diligence in researching treatment options available to them; this is because many patients simply find themselves on the traditional path of treatment and are unaware of other options.
For those on the traditional path of scoliosis treatment, there is a lot of watching and waiting, commonly followed by a surgical recommendation.
For those who choose to forgo a surgical recommendation, or who simply want to explore less-invasive treatment options first, the Scoliosis Reduction Center® has many beneficial treatment goals: impacting the condition on a structural level in the form of a curvature reduction, increasing core strength so the spine is optimally supported, preserving the spine’s overall health and function, and avoiding the need for invasive surgery.
If you, or someone you care about, has recently been diagnosed with scoliosis, the time to start treatment is always now, and reaching out to us here at the Center can be the first step on the road to treatment success.





