Officially known as spinal fusion, scoliosis surgery has the end goal of stopping progression, but that’s not the same as working towards achieving corrective results that involve a curvature reduction and increasing core strength for improved spinal support.
Scoliosis is a complex spinal condition, and there are different ways to treat it that offer patients different potential outcomes. A traditional surgical approach can cost the spine in terms of its overall strength and function, while a conservative approach offers a nonsurgical treatment alternative.
Before getting to the specifics of spinal fusion surgery, let’s start with some important condition characteristics.
4 Key Takeaways
- Scoliosis Defined: Scoliosis is a structural condition characterized by an abnormal lateral spinal curvature with rotation, diagnosed through a Cobb angle of at least 10 degrees. Its progressive nature underscores the importance of proactive treatment.
- Spinal Fusion Surgery: Spinal fusion aims to halt scoliosis progression by fusing the curve’s most-tilted vertebrae into a solid bone, utilizing hardware to maintain alignment. While it can stop progression, it may also limit spinal flexibility and range of motion, highlighting the need for careful consideration.
- Surgery Success and Risks: While spinal fusion can be effective in preventing curve progression, the risks and potential for complications, including failed back surgery syndrome, suggest that success is not guaranteed and subsequent surgeries may offer diminishing returns.
- Conservative Treatment Alternatives: A conservative, chiropractic-centered approach offers a nonsurgical alternative focused on correcting the curvature and enhancing spinal support without sacrificing flexibility and range of motion. This approach integrates chiropractic care, physical therapy, corrective bracing, and customized exercises for comprehensive treatment.
What is Scoliosis?
Scoliosis is a structural spinal condition that involves the development of an unnatural lateral (sideways) spinal curve.
Not only does a scoliotic curve bend unnaturally to the side, it also twists, and it’s the rotational component that makes scoliosis a 3-dimensional condition, so in order for treatment to be effective, it has to address it as such.
In addition, a scoliotic curve has to be of a minimum size to be officially diagnosed as scoliosis: a Cobb angle measurement of at least 10 degrees.
A patient’s Cobb angle is taken during X-ray by drawing lines from the tops and bottoms of the curve’s most-tilted vertebrae; the intersecting angle is expressed in degrees.
Cobb angle tells me how far out of alignment a scoliotic spine is, in addition to placing conditions on a severity scale:
Mild scoliosis: Cobb angle measurement of between 10 and 25 degrees
Moderate scoliosis: Cobb angle measurement of between 25 and 40 degrees
Severe scoliosis: Cobb angle measurement of 40+ degrees
Very-severe scoliosis: Cobb angle measurement of 80+ degrees
Cobb angle is known as the gold standard in the assessment of scoliosis, and when it comes to scoliosis surgery, a patient’s Cobb angle is a key factor because when it progresses to a certain point, this is when patients are commonly funneled towards spinal fusion surgery, at least for those on the path of traditional scoliosis treatment.
As a progressive condition, scoliosis has it in its nature to worsen over time; only proactive treatment can counteract this tendency, and this is why how a condition’s diagnosis is responded to is so important when it comes to maintaining a positive scoliosis quality of life.
So for those on the path of traditional treatment, what can they expect?
Spinal Fusion Surgery
While there are different types of spinal fusion, the procedure generally entails fusing the unnatural spinal curve’s most-tilted vertebrae into one solid bone, and this is to eliminate movement (progression) so those vertebrae can’t become more tilted over time.
This also involves the removal of intervertebral discs that sit between adjacent vertebrae being fused, and in most cases, rods are attached to the spine with screws to hold it in place.
The spine’s intervertebtral discs give the spine structure (adjacent vertebrae attach to the disc in between), enable spinal flexibility and range of motion, and act as the spine’s shock absorbers.
The health of the spinal discs are a crucial element in maintaining overall spinal health, so their removal doesn’t come without a cost.
In addition, making one section of the spine immoveable is contrary to its movement-based design, and can cost patients in terms of spinal flexibility and range of motion.
A spine that’s fused is also not as strong so is going to be more vulnerable to injury.
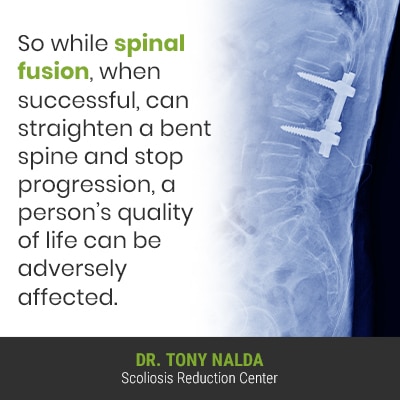
So while spinal fusion, when successful, can straighten a bent spine and stop progression, a person’s quality of life can be adversely affected.
Scoliosis Surgery Success Rate
For those considering back surgery, and specifially spinal fusion surgery, failed back surgery syndrome (FBSS) is a growing issue.
If a patient is to undergo spinal fusion to treat their scoliosis, and for a number of reasons, it’s unsuccessful, the only recourse is more surgery, and with each additional spinal surgery, the risks increase, and the chances of a successful outcome decrease.
Although it’s estimated that approximately 60 to 80 percent of primary spinal surgeries have successful results, it’s estimated that no higher than 30, 15, and 5 percent of patients will experince another successful outcome after their second, third, and fourth spinal surgery; 20-40 percent of spinal surgeries are unsuccessful at improving the health of the spine.
The older a patient is, the more risky surgery is, so for adults with scoliosis, spinal fusion becomes increasingly risky with age, and with each subsequent surgery, so spinal fusion in the treatment of adult scoliosis also has to be considered carefully.
Not everyone will experience the side effects and complications of spinal fusion, but the risks are there, so should be considered carefully, and the way the spine is held in place by artificial means can cost the spine in terms of its strength, flexibility, and range of motion.
Scoliosis Surgery Alternatives
For those choosing to forgo a surgical recommendation, or for those who want to try a less-invasive treatment alternative first, there is a nonsurgical treatment alternative with proven results.
Here at the Scoliosis Reduction Center®, I want to help patients work towards preventing progression through a conservative chiropractic-centered treatment approach that strives to preserve as much of the spine’s natural function as possible.
I don’t value a huge curve reduction over function; I’d rather reduce a curve as much as possible, while preserving the spine’s natural flexibility and range of motion; that gives patients the best scoliosis quality of life.
While traditional treatment that funnels patients towards spinal fusion opts for watching and waiting until a condition becomes severe, making the patient a surgical candidate, I value starting proactive treatment as close to the time of diagnosis as possible; that way, valuable treatment time isn’t being wasted.
While there are no treatment guarantees, early detection, when responded to with proactive treatment, increases the chances of treatment success.
Conservative Chiropractic-Centered Treatment
By integrating multiple forms of treatment such as chiropractic care, physical therapy, corrective bracing, and custom-prescribed home exercises, conditions can be impacted on every level.
As a 3-dimensional structural spinal condition, scoliosis has to be impacted primarily on a structural level, and this is worked towards through condition-specific chiropractic care; a series of chiropractic techniques and manual adjustments can work towards repositioning the most-tilted vertebrae of the curve back into alignment with the rest of the spine.
By addressing any areas of vertebral subluxation through chiropractic care, the spine’s alignment and natural curves are being restored.
Through physical therapy, I can help patients work towards increasing core strength so the spine can be better supported by its surrounding muscles; after all, it’s not just the spine that has to maintain its natural curves and alignment, but also its surrounding muscles.
Through corrective bracing, I can augment corrective results achieved through other treatment disciplines by pushing the spine into a corrective position, and corrective bracing like the ScoliBrace acknowledges the condition’s 3-dimensional nature, so addresses its rotational component, which traditional scoliosis bracing does not, (one of the reasons why its efficacy is limited).
Through a series of custom-prescribed exercises and stretches, I can help patients establish a home-rehabilitation program to further stabilize the spine.
The bottom line is that there are different ideals of what constitutes successful treatment results, and when it comes to scoliosis surgery success, while stopping progression and straightening the spine is within the scope of spinal fusion, it can cost the spine when it comes to its strength, flexibility, and range of motion.
Conclusion
For patients recently diagnosed with scoliosis, the most important decision moving forward is how to treat it, and this is because different treatment approaches offer patients different potential outcomes.
Those who undergo spinal fusion need to be aware of the procedure’s potential risks, side effects, and complications because once the spine is fused, it’s fused for life; if the surgery is unsuccessful at stopping the condition from progressing, the only recourse is more surgery, and success rates decrease with each additional procedure.
For those looking for a more natural treatment approach, a conservative chiropractic-centered treatment approach offers a nonsurgical alternative that relies on integrating multiple forms of treatment, all with corrective potential, into fully-customized treatment plans.
While spinal fusion, when successful, can still cost the spine in terms of its overall health, strength, and function, a conservative treatment approach preserves as much of the spine’s natural function as possible by impacting the condition, first and foremost, on a structural level for true corrective results.
As a progressive spinal condition, it’s virtually guaranteed to worsen over time, so treatment that’s started early in a condition’s progressive line has the best chance of preventing progression, increasing condition severity, escalating symptoms, and the need for invasive surgical treatment in the future.




