Scoliosis Treatment Approach
Why Our Scoliosis Treatment Approach Is Different
As opposed to just trying to hold the spine with a brace or rod, we utilize a more natural, functional approach that strengthens the spine so it can begin to support itself. By strengthening the spine in a corrective position, it becomes more resistance to scoliosis progression. This approach can normally involve multiple types of treatment such as chiropractic, exercise therapy, active rehabilitation, passive rehabilitation, and corrective bracing. Adolescent idiopathic scoliosis is a common type of scoliosis that benefits from this approach, but our approach works for many other types of scoliosis as well.


The problem lies in that patients must go to multiple clinics, offices, doctors and therapist to receive all these types of treatment. This is where our training comes in. We have received multiple treatment certifications that encompass all of these approaches in one setting so everything works in unison. Our methods include conservative scoliosis treatment options tailored for idiopathic scoliosis and other types, ensuring comprehensive care.
Rehabilitation using these types of treatments involve patients being seen 3 times a week for 12 to 16 weeks. At that point, post evaluations are done to determine if any results were achieved. This approach works great for most conditions like injuries, pain, disc problems, etc… However, for scoliosis, this slow, gradual recommendation normally doesn’t have the ability to overcome the complexity, rigidity, and progressive nature of scoliosis. Our treatment aims to prevent curve progression, which is crucial for effective scoliosis management.
We have designed programs understanding that scoliosis rehabilitation cannot be like traditional rehabilitation for it to be effective. Our treatment options condenses the duration and increases the intensity of the treatment. This intensive formula is what provides the ability to overcome the progressive nature of scoliosis. Intensive does not mean painful; it simply means lots of treatment in a short period of time. Pain management, through mobility and flexibility exercises, is also a key component of our approach to ensure patient comfort.
After the office treatment is received, patient’s will receive an individualized home program to sustain the results achieved. This approach is what allows patients of all ages, and from all over the world to achieve results they thought were not possible with traditional treatment options. Patient age is a significant factor in determining the treatment plan, as it influences the rate of condition progression, but we can provide treatment for all ages.
Our comprehensive approach to scoliosis treatment methods not only addresses the physical aspects but also significantly improves the quality of life for our patients.
Scoliosis-Specific Chiropractic
Traditional chiropractic has had mixed results in scoliosis, with little benefit found to the practices employed by most chiropractors, even in mild cases. However, more advanced and scoliosis-specific techniques can be more effective in treating scoliosis, just like scoliosis-specific exercises are more effective than general physical therapy. Scoliosis specific chiropractic differs not only in the frequency of treatment, duration of treatment, but in the actual chiropractic treatment delivered to the patient.
CLEAR™ scoliosis treatment is different from traditional chiropractic care for scoliosis. Our approach was designed specifically to help people with scoliosis. Our methods have been in clinical use since 2000 in chiropractic offices around the world, and our treatment protocols are taught in the postgraduate curriculum of accredited chiropractic universities. To ensure patient safety and optimal outcomes from care, CLEAR™ scoliosis treatment can only be provided by CLEAR™ certified chiropractors. Our treatment is tailored to address various scoliosis curves, ensuring effective management and correction on the severity of the condition.
Scoliosis-Specific Exercises

Scoliosis-specific exercises, sometimes called SSE’s, have been gathering increasing evidence for effectiveness. Most of these SSE techniques arose in Europe, and are now beginning to find their way over to the US, Asia, Australia, and elsewhere. Scoliosis-specific exercises are self-correction exercises that are customized for every patient based upon ability and curve type. These exercises consist of a combination of active movement based exercise, isometric exercises, and reflexive exercises.
One effective exercise approach is the Schroth method, which has shown significant results in scoliosis treatment.
One exercise approach we are certified in is SEAS. SEAS is the acronym for “Scientific Exercise Approach to Scoliosis.” SEAS is based on a specific active self-correction technique performed without external aid, and incorporated in functional exercises. Improvement of the stability of the spine in active self-correction is the primary objective of SEAS. SEAS exercises train neuromotor function so to stimulate by reflex a self-corrected posture during the activities of daily life. This method is part of the broader category of scoliosis specific exercises.
In addition, CLEAR™ utilizes its own unique scoliosis specific exercise program. These involved customized exercises influence posture, balance, and coordination. A CLEAR™ doctor will prescribe customized equipment that will be used to achieve a reflexive response with a scoliosis patient. The most neurological type of exercise is one that incorporates the use of a person’s reflexes and requires no conscious contraction. We have designed a customized exercise program and the equipment needed to achieve this type of exercise; where other approaches mostly focus on conscious exercise only.
Scoliosis-Specific Therapy
Scoliosis-specific therapy has one goal in mind, to passively mobilize the spine into a corrected position. This type of treatment includes multiple types of treatment such as vibration, traction and de-rotation. Normally this is achieved using multiple types of equipment specially designed to reduce a scoliosis. Additionally, managing spinal deformity (reducing the curve) through specific therapeutic methods is crucial for effective treatment.
One such device is a Scoliosis Traction Chair. The idea behind the scoliosis traction chair is simple, to reverse a case of scoliosis into a mirror-image of itself. The Scoliosis Traction Chair is only one part of the CLEAR™ Scoliosis Treatment Protocols. Each part of the treatment is intended to complement the others.
Since the Scoliosis Traction Chair has been shown to be effective in mirroring imaging the scoliosis this has led to other device to be created. Devices like a scoliosis flexion distraction table, a thoracic mechanical drop piece, vibrating cervical traction, and others, have been designed to be used in combination to achieve the most desirable results with our scoliosis-specific therapy. These scoliosis treatment methods align with SOSORT guidelines, focusing on improving spinal stability, enhancing postural balance, and addressing aspects related to bracing.
Scoliosis Is Not 2D, But 3D
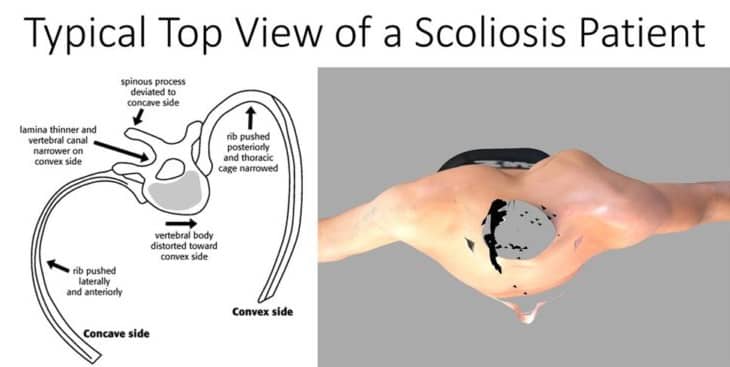
As you can see below, scoliosis is not a 2-dimensional problem that only consist of lateral bending of the spine, but it is actually a 3-dimensional problem. This top view of a scoliosis patient shows how the torso/ribs and spine rotate as well as bend.
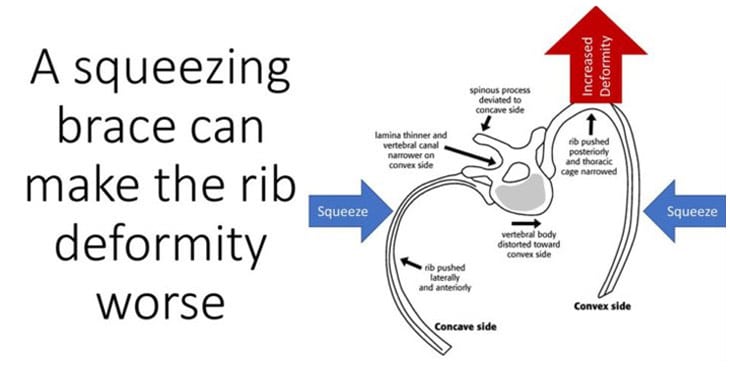
Typical Boston braces don’t address the rotational component of scoliosis because they only squeeze the body from the sides. In fact, squeezing from the sides can increase rotation while attempting to control lateral spine bending.
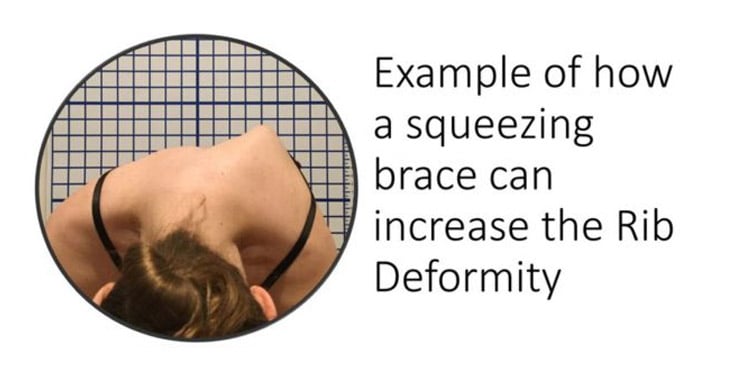
Below is an example of a patient that wore a typical squeezing style Boston brace. Here you can see how the rib deformity has become more pronounced and pointier in nature. Unfortunately, this is a common consequence of a brace that squeezes.
Not All Scoliosis Braces Are The Same
What makes a brace effective in the reduction of scoliosis is the design. The design of the scoliosis brace will determine how the brace functions. A poorly designed scoliosis brace will never produce a good result and can hinder the effectiveness of other treatments like exercise, therapy, chiropractic and rehabilitation. However, a properly designed scoliosis brace can do the opposite. One key measurement is in brace correction on x-ray. The better in-brace correction, typically, the better results.
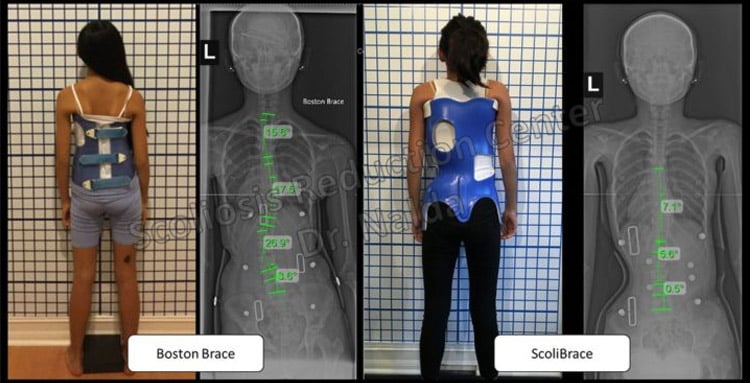
In this picture, the example on the left side, you can see an example of a patient that was prescribed a Boston brace.
The Boston brace was built to squeeze the spine with attempt to just try to hold the spine from getting worse.
The photo on the right shows the same patient in a corrective brace that pushes and doesn’t squeeze.
The in-brace correction comparison is obvious in which brace is going to be more effective in the reduction of the scoliosis.
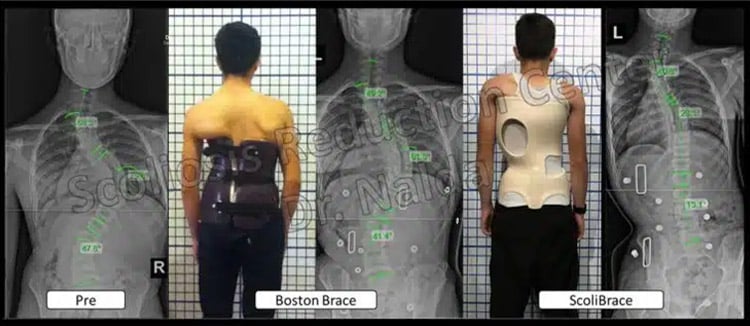
Here is another example of the limitation of squeezing.
Even large curves can respond to a properly designed brace.
The in-brace correction is 40 degrees better in the corrective brace versus the Boston brace, showing the ineffectiveness of squeezing braces.
A Providence brace is another type of a common brace used. Providence braces are also referred to as “nighttime bending braces.” Due to design, the brace can only be worn during sleeping hours. Even though these tend to show a better in-brace correction, they are limited on the reduction they can achieve because they only laterally bend the spine, and they can only be used for a limited time.
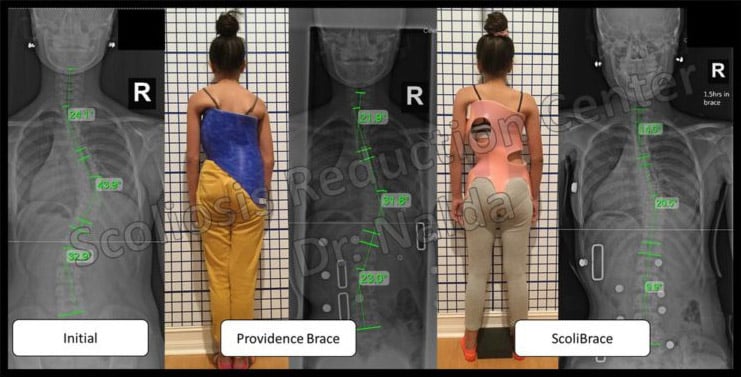
Here is an example of a patient that was initially prescribed a Providence brace and progressed to 43 degrees while under brace treatment. At that time was recommended surgery. You can see the second photo shows the Providence brace and how it achieves a decent in-brace correction. However, since the brace can only be worn for 8 to 10 hours it has failed in stopping progression of this case. The photo on the right shows how a properly designed corrective brace can produce better in brace correction, while the patient is able to maintain longer in brace time and will ultimately produce better results.
Super-Corrective Scoliosis Braces
By positioning the body and spine in their over-corrected or mirror image position, the ScoliBrace® can have a super-corrective effect. Curve reductions are achieved in the majority of cases, as well as improvements to rib humping, shoulder level and the overall appearance of the body.
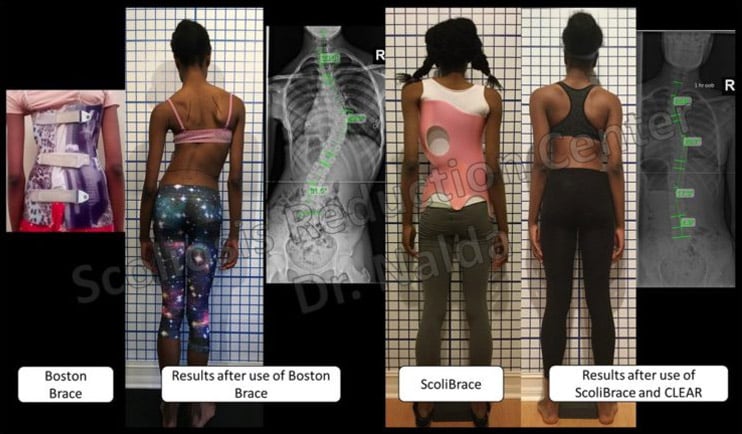
Here is an example of a patient that wore a Boston brace for years.
The 1st photo shows her brace fit, notice how the brace just squeezes her.
The second photo shows the results after her wearing the Boston brace; at this point she was scheduled for surgery. Spinal fusion is a common surgical option in such cases, aiming to halt curve progression and minimize complications, though it is risky and it limits the spine’s flexibility and overall function.
The third photo shows how a properly designed corrective brace pushes instead of squeezes.
The last photo shows the results of a complete corrective program, which includes a combined treatment of corrective bracing, exercise, therapy and chiropractic. The results are dramatically different.

3D Brace for a 3D Condition
Scoliosis is a 3 dimensional condition. Effective treatments need to be 3 dimensional too. ScoliBrace® is created from 3D bodyscans in conjunction with x-rays and posture photos.
Each brace is then designed using Computer Aided Design (CAD) software and custom made.
We believe our brace design, manufacturing and correction is superior to any standard brace available today.
Ready to get started?
This course of treatment works great for all scoliosis severities: mild, moderate, and severe. Whether you think you are ready to start treatment for scoliosis or you have further questions, the next step is to reach out to us. Click the button below to get in touch with us or call us at 321-939-2328.
Contact Us Today