In order for structural scoliosis to be given as a diagnosis, certain condition characteristics have to be met. Structural scoliosis involves having an abnormal sideways curvature to the spine, but that curvature has to be of a certain size, and there has to be rotation present. In addition, scoliosis radiography tells us what we need to know to design an effective treatment plan moving forward, such as the type and location of the curvature.
Scoliosis X-rays remain the gold standard for diagnosing, assessing, and monitoring scoliosis. They tell us how much a scoliotic spine deviates from a straight alignment via a measurement known as ‘Cobb angle’, if there is rotation present, and if the condition fulfills the definition of structural scoliosis.
When it comes to a progressive spinal condition like scoliosis, in addition to diagnosing and assessing it, monitoring the spine throughout treatment, as needed, to see how it is responding is very important. Before we move on to the specifics of scoliosis X-rays and what they can tell us, let’s first talk generally about scoliosis.
What it Means to Have Scoliosis
As mentioned, scoliosis means having an abnormally-curved spine. While a healthy spine has natural curvatures that give it added strength, flexibility, and help it distribute mechanical stress throughout, an unhealthy spine can develop unnatural curvatures that disrupt the spine’s biomechanics and overall function.
When scoliosis develops, the spine abnormally curves to the side, and if certain condition characteristics are met, a diagnosis of structural scoliosis is given. There is a difference between nonstructural and structural scoliosis as the former is temporary, commonly caused by bad posture, and the curvature does not involve rotation: a key element of scoliosis.
Now, let’s move on to the parameters that have to be met for a structural scoliosis diagnosis to be given, and the role that X-rays play. Recent innovations in scoliosis imaging, such as low-dose 3D imaging and cone-beam CT, provide clearer, detailed images of the spine, aiding healthcare providers in creating personalized treatment plans.
Types of Scoliosis
Scoliosis is a complex condition that can manifest in various forms, each with distinct characteristics and implications for diagnosis and treatment. The main types of scoliosis include:
- Idiopathic Scoliosis: This is the most common form of scoliosis, accounting for approximately 80% of cases. It is characterized by an abnormal lateral curvature of the spine, with no identifiable cause. Idiopathic scoliosis can occur at any age, but it is most commonly diagnosed in adolescents. This type of scoliosis often requires careful monitoring and a tailored treatment plan to manage its progression effectively.
- Congenital Scoliosis: Present at birth, congenital scoliosis is caused by abnormalities in the development of the spine during fetal growth. These abnormalities can lead to a range of spinal deformities, which may be associated with other birth defects. In many cases, congenital scoliosis may require surgical intervention to correct the spinal curvature and prevent further complications.
- Neuromuscular Scoliosis: This type of scoliosis is caused by neurological or muscular disorders, such as muscular dystrophy, cerebral palsy, or spina bifida. Neuromuscular scoliosis can lead to severe spinal deformities and may significantly impact a patient’s quality of life. Treatment often involves a combination of bracing, physical therapy, and sometimes surgery to manage the condition and improve mobility.
- Degenerative Scoliosis: Occurring in adults, degenerative scoliosis is caused by age-related changes in the spine, such as osteoporosis, disc degeneration, or spinal stenosis. This type of scoliosis can lead to back pain, stiffness, and limited mobility. Treatment typically focuses on pain management, physical therapy, and in some cases, surgical intervention to alleviate symptoms and improve spinal alignment.
Diagnosing Scoliosis
When a young patient comes to see me with concerns about scoliosis, it’s often because a routine physical has spotted an abnormal spinal curvature.
While scoliosis is incurable and progressive, it is highly treatable, but before the first steps on the road to treatment can be taken, I need accurate assessment and measurements, and this is achieved with the scoliosis X-ray, while also considering the importance of minimizing ray exposure.
While scoliosis can develop at any age and take many forms, the most prevalent condition type is adolescent idiopathic scoliosis (AIS) diagnosed between the ages of 10 and 18.
To officially diagnose scoliosis, I conduct a physical exam with many tests, including taking the patient’s medical history and watching how they walk; I can tell a lot about a patient’s condition by how they walk.
Often, the asymmetries produced by scoliosis are more noticeable when in a forward-bend position. If I see indicators for the condition, a scoliosis X-ray is the next step to reaching a diagnosis.
Often, the asymmetries produced by scoliosis are more noticeable when in a forward-bend position. If I see indicators for the condition, a scoliosis X-ray is the next step to reaching a diagnosis.
What a Scoliosis X-ray Can Tell Us
A scoliosis X-ray can tell us what we need to know about a condition to treat it effectively. It tells us if the abnormal spinal curvature includes rotation, how severe the curvature is, what type of curvature it is, and where along the spine the curvature has developed, including the thoracic spine.
For an official scoliosis diagnosis to be given, there has to be rotation, and the curvature has to have a minimum measurement of 10 degrees.
Cobb angle is measured by drawing intersecting lines from the tops and bottoms of the curvature’s most-tilted vertebrae, and the resulting angle is measured in degrees.
A patient’s Cobb angle is one of the most important pieces of information; it gives us a starting point from which we can monitor treatment progress and places the condition on its severity scale of mild, moderate, severe, or very severe.
- Mild scoliosis: Cobb angle measurement of between 10 and 25 degrees
- Moderate scoliosis: Cobb angle measurement of between 25 and 40 degrees
- Severe scoliosis: Cobb angle measurement of 40+ degrees
- Very-severe scoliosis: Cobb angle measurement of 80+ degrees
As scoliosis is progressive, this means its nature is to worsen over time, especially if left untreated.
Placing a condition on its severity scale, plus other condition characteristics such as curvature location and type, help us predict a patient’s likeliest rate of progression; I say ‘likeliest’ because there is no way to predict, with 100-percent accuracy, how much or how quickly a patient’s condition will progress.
Certain curvature patterns, such as thoracic curves, tend to progress faster, so knowing the location of the curvature along the spine can give us more progression-related guidance.
X-ray images can also tell us if a scoliosis is considered typical or atypical; most scoliosis curvatures bend to the right, away from the heart, but if an X-ray shows a curvature bending to the left, towards the heart, this tells me it is an atypical case, likely with another condition/disease causing the scoliosis as a secondary complication.
Every case of scoliosis is different, which is why a customized treatment approach is so important. For a treatment plan to be effective, it has to address the specifics of each patient and their condition, which is why X-ray results are so important.
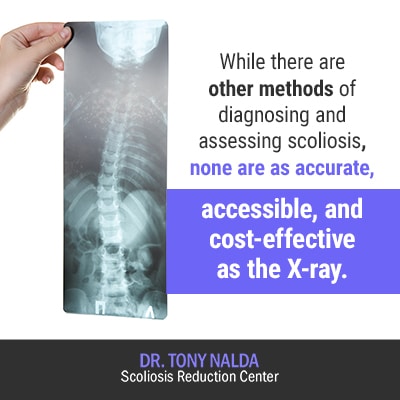
While there are other methods of diagnosing and assessing scoliosis, none are as accurate, accessible, and cost-effective as the X-ray.
It is extremely important, however, that the practitioner performing the X-ray has the scoliosis-specific training, experience, and knowledge to interpret the results of the 3-dimensional condition so an effective treatment plan can be crafted.
Reading 2-Dimensional Images of a 3-Dimensional Condition
Scoliosis is a 3-dimensional condition, meaning it doesn’t just bend to the side, but also twists, which is the rotation factor.
In order for the condition to be impacted on a structural level effectively, it has to be treated as a 3-dimensional condition, which is why it’s so important to be able to conduct and read a scoliosis X-ray comprehensively.
While traditional X-rays provide 2-dimensional images, experts who specialize in scoliosis understand how to use multiple X-rays to construct a complete picture of the spine from side to side, front to back, and back to front, including clear images of the lumbar spine to ensure accurate diagnosis and effective treatment planning.
Without the proper expertise, the proper measurements needed to treat scoliosis effectively can’t be taken, and this can impact treatment efficacy, which is why it’s so important to enlist the help of a practitioner who specializes in scoliosis.
When scoliosis patients come to see me here at the Scoliosis Reduction Center®, I use multiple measurements to assess their condition. By looking at the spine from several different angles, I can measure twist, tilt, and other important factors.
There is more to measuring scoliosis than just the Cobb angle, and crafting an effective treatment plan is only possible when the condition is assessed from all angles.
Advancements in Scoliosis Diagnosis with 3D X-Ray Imaging and Minimal Radiation Exposure
X-ray imaging has long been a cornerstone in diagnosing and managing scoliosis, offering critical insights into the condition of the spine. Traditional two-dimensional X-rays provide valuable information about the curvature’s degree and location. However, scoliosis is inherently a three-dimensional deformity, involving not just lateral curvature but also rotational aspects of the vertebrae. This is where 3D X-ray imaging has revolutionized scoliosis assessment, offering a more comprehensive view of the spinal anatomy.
When a patient undergoes a 3D scoliosis X-ray, doctors can visualize the spine from multiple angles, capturing the complexities of the curvature and vertebral rotation with greater precision. This advanced imaging technique allows for more accurate measurement of the Cobb angle, which quantifies the degree of spinal curvature. By assessing the spine in three dimensions, physicians can better understand the exact nature of the deformity, including the rotational component that contributes to rib prominence and asymmetry.
3D X-ray imaging enhances the ability to detect other spinal abnormalities that may accompany scoliosis. For instance, congenital anomalies like hemivertebrae—where only half of a vertebra forms—are more readily identified with three-dimensional views. Additionally, signs of degenerative changes in adults, such as disc degeneration or bone spurs, can be evaluated more thoroughly. Identifying these factors is crucial for a comprehensive assessment and for tailoring a treatment plan that addresses all aspects of the patient’s spinal health.
Another significant advantage of 3D X-rays is in treatment planning and monitoring. With a detailed three-dimensional model of the spine, orthopedic specialists can design more effective bracing strategies that conform precisely to the patient’s anatomy. For surgical candidates, 3D imaging assists in preoperative planning, allowing surgeons to anticipate challenges and optimize surgical approaches. Post-treatment, 3D X-rays enable precise monitoring of spinal changes over time, ensuring that interventions are achieving the desired outcomes.
While radiation exposure is a concern with any X-ray procedure, modern 3D imaging systems often incorporate technologies that reduce dose without compromising image quality. Techniques such as EOS imaging use low-dose radiation to produce high-quality 3D images, making them suitable for repeated use, especially important in monitoring adolescent patients during growth spurts.
In summary, 3D X-ray imaging has become an invaluable tool in the diagnosis and management of scoliosis. By providing a complete and detailed visualization of the spine’s structure, it allows for more accurate assessments, personalized treatment plans, and effective monitoring of the condition’s progression. This advanced imaging technology ultimately contributes to improved patient outcomes, helping those with scoliosis achieve better spinal alignment, reduced discomfort, and an enhanced quality of life.
How to Read a Scoliosis X-Ray
Here at the Center, we rely on X-rays every day to diagnose, assess, and manage our patients’ scoliosis, when necessary, but there are a few things that set us apart:
 We use the most advanced digital scoliosis X-ray technology to give us the greatest accuracy with the least amount of radiation exposure.
We use the most advanced digital scoliosis X-ray technology to give us the greatest accuracy with the least amount of radiation exposure.- We use small, specifically-targeted X-rays to assess the biomechanical integrity of the spine and gain more precise measurements.
- As my focus is scoliosis, I’ve measured thousands of scoliosis X-rays and have the ability to craft more precise, patient-specific, and effective treatment plans.
- I use scoliosis X-rays throughout treatment, when needed, to gauge progress, apply specific targeted chiropractic adjustments, prescribe scoliosis-specific exercises, and make sure a patient’s condition is being treated in the most effective and efficient manner possible.
While not necessary for every patient, I also have access to Digital Motion X-ray, which can be helpful in isolating and assessing the source of spinal instability and scoliosis-related pain during movement.
Digital Motion X-Ray
In addition to traditional static X-ray, I also utilize Digital Motion X-ray when an individual case necessitates it.
Digital Motion X-ray (DMX) is a medical-imaging technology that can visualize the body while in motion, providing video images of how the bones are engaged during movement. This is particularly beneficial for patients who are experiencing a lot of pain and isolating its source.
DMX is an innovative diagnostic tool that can be used to visualize all joints in the body during real-time motion. DMX can reveal spinal instability, and as joint-related pain is generally at its worst during motion, having scans produced while a patient is experiencing symptoms can help me design the most effective treatment plan for addressing those symptoms.
DMX offers excellent resolution and a large dynamic range, allowing for complete and precise measurements used in orthopedic applications.
However, the use of DMX for every patient is unnecessary because as a CLEAR-certified scoliosis chiropractor following the CLEAR approach, I take approximately 77 different measurements via static X-ray, which is far more than what a general chiropractor or medical doctor is assessing.
As my focus is scoliosis, I have the knowledge and ability to utilize standard 2-dimensional X-ray images in such a way that I can fully construct a 3-dimensional picture of what is happening with the spine and design an effective and customized treatment plan moving forward.
While there are a number of screening and assessment methods used for scoliosis, X-rays provide the most safe, reliable, accessible, and cost-effective means of doing so.
Scoliosis X-ray results tell me everything I need to know about a patient’s condition to treat it effectively. While scoliosis is a 3-dimensional condition and standard X-rays produce 2-dimensional images, I have the scoliosis-specific certifications, experience, and knowledge to interpret the images comprehensively, in order to provide patients with the best information and most effective treatment plans.
Not only does performing scoliosis X-rays, when needed, allow me to effectively identify the condition, they provide me with enough information to craft an effective treatment plan, and the means by which I can monitor how the spine is responding to treatment.
The important thing to remember, when it comes to scoliosis X-rays, is that the information they provide can only be shaped into effective treatment plans if the spine is being looked at from multiple angles, addressing the condition’s 3-dimensional nature.
Here at the Scoliosis Reduction Center®, we have access to the latest X-ray technology and take measurements of the spine from several different angles to measure twist, tilt, and other important condition characteristics.
Monitoring Progression
Monitoring the progression of scoliosis is crucial for effective management and treatment. Regular check-ups with a healthcare provider, including X-rays and physical examinations, can help track changes in the spinal curvature and detect any potential complications. The frequency of monitoring depends on the severity of the scoliosis, the patient’s age, and the treatment approach.
- X-ray evaluation: Regular scoliosis x-rays are essential for monitoring the progression of scoliosis. These X-rays can help measure the Cobb angle, identify spinal and rib deformations, and monitor changes in the curvature over time. By comparing X-ray images taken at different intervals, healthcare providers can assess how the condition is evolving and adjust treatment plans accordingly.
- Physical examination: A thorough physical examination can help assess the patient’s overall health, detect any changes in the spinal curvature, and evaluate the effectiveness of treatment. During these exams, healthcare providers may look for signs of asymmetry, changes in posture, and other physical indicators of scoliosis progression.
- Scoliometer measurements: A scoliometer is a device used to measure the degree of spinal curvature. Regular scoliometer measurements can help track changes in the curvature and detect any potential progression. This non-invasive tool is often used in conjunction with X-rays to provide a comprehensive assessment of the condition.
Scoliosis X-Ray Techniques and Safety
Scoliosis X-rays are a crucial diagnostic tool for evaluating and monitoring scoliosis. However, concerns about radiation exposure have led to the development of safer X-ray techniques and safety measures.
- Low-dose radiation: Modern X-ray machines use low-dose radiation to minimize exposure. The Health Physics Society recommends that X-ray doses be kept as low as reasonably achievable (ALARA) to minimize radiation exposure. This approach ensures that patients receive the necessary diagnostic information while reducing the risk associated with radiation.
- EOS imaging system: The EOS imaging system is a low-dose X-ray system that uses a biplanar X-ray device to capture images of the entire spine. The EOS system reduces radiation exposure by up to 90% compared to traditional X-ray systems. This advanced technology provides high-quality images with minimal radiation, making it an excellent option for monitoring scoliosis, especially in children and adolescents.
- Shielding: Shielding is used to protect sensitive areas, such as the breasts and ovaries, from radiation exposure. Lead aprons and thyroid shields are commonly used to minimize radiation exposure. These protective measures are essential for ensuring patient safety during X-ray procedures.
- Positioning: Proper positioning is essential for accurate X-ray images. Patients should be positioned in a way that minimizes radiation exposure and ensures accurate measurements. Correct positioning helps capture the necessary views of the spine while reducing the need for repeat X-rays.
Minimizing Radiation Exposure
Minimizing radiation exposure is essential for patients with scoliosis, particularly children and adolescents. The following measures can help reduce radiation exposure:
- Use low-dose X-ray machines: Modern X-ray machines use low-dose radiation to minimize exposure. These machines are designed to provide high-quality images with the least amount of radiation necessary.
- Optimize X-ray techniques: X-ray techniques can be optimized to reduce radiation exposure, such as using the lowest possible dose and minimizing the number of X-rays taken. This approach ensures that patients receive the necessary diagnostic information with minimal radiation.
- Use shielding: Shielding can be used to protect sensitive areas from radiation exposure. Lead aprons, thyroid shields, and other protective devices are essential for minimizing radiation exposure during X-ray procedures.
- Monitor radiation exposure: Radiation exposure should be monitored and recorded to ensure that patients receive the minimum necessary dose. Keeping track of cumulative radiation exposure helps healthcare providers make informed decisions about the frequency and necessity of X-ray imaging.
By implementing these measures, healthcare providers can effectively minimize radiation exposure while still obtaining the critical information needed to diagnose and monitor scoliosis.