Mild Scoliosis
Early Stage Intervention Is So Important
Part of diagnosing a patient with scoliosis is further classifying the condition. This is based on various characteristics of the condition and the patient such as age, cause (if known), condition severity, and location of the curvature. Once a patient’s condition is classified as mild, moderate, or severe, we can move forward with designing a customized treatment plan.
When a person first receives a scoliosis diagnosis, that diagnosis includes a classification of the condition. Based on a measurement known as ‘Cobb angle’, the patient’s scoliosis is classified as mild, moderate, or severe. If a patient’s spine bends and rotates with a Cobb angle measuring between 10 and 25 degrees, this is considered ‘mild scoliosis’.
If you or a loved one has recently been diagnosed with mild scoliosis, chances are, the patient will be feeling anything but lucky; however, just by detecting the condition in its mildest form, they are already ahead of the game. This is because when it comes to the condition’s most common form, early detection can be as challenging as it is beneficial.
What Is Mild Scoliosis and How is it Classified?
The human spine has three main natural healthy curves. These curves give the spine its strength, flexibility, and allow us to maintain an upright posture.
If there is a loss of one or more of those healthy curves, the spine’s overall biomechanics are thrown off, and this can lead to a number of experienced symptoms and potential complications.
If a spine has an abnormal bend to the side, plus has rotation, these are good indicators that scoliosis is present.
The other marker that has to be met is what’s known as ‘Cobb angle’.
Cobb Angle
The Cobb angle is a measurement, taken via X-ray, from the most-tilted vertebrae of the curvature; this measurement tells us how far from a natural and healthy alignment the patient’s spine twists and bends. If the Cobb angle measures more than 10 degrees but less than 25 degrees, this is classified as ‘mild scoliosis,’ which is the first stop on the condition’s progressive line.
While the Cobb angle is a crucial part of classifying scoliosis, other important factors include the patient’s age, the condition’s cause (if known), and the location of the curvature.
Patient’s Age
While scoliosis can develop at any age, its most common form develops between the ages of 10 and 18: adolescent idiopathic scoliosis (AIS). This form of the condition makes up 80 percent of known diagnosed cases.
Age is significant because it indicates a patient’s fitness level and ability to handle treatment. Age also matters because skeletal maturity removes the biggest trigger for progression: growth. Younger patients, still growing, are at the highest risk of progression. Additionally, age can hint at likely symptoms, such as pain, making early detection crucial yet challenging.
Condition Cause
The most common form of scoliosis is AIS, which means there’s no single known cause for the condition’s onset. Instead, AIS is thought to develop from multiple factors that vary among patients. AIS makes up 80 percent of known cases. The remaining 20 percent have known causes, including neuromuscular, congenital, degenerative, and traumatic scoliosis.
These forms of scoliosis develop as secondary complications to primary medical issues or diseases, requiring treatment that addresses the underlying medical condition first and foremost.
Location of the Curvature
There are three main sections to the spine: cervical (upper back and neck), thoracic (middle back), and lumbar (lower back). Scoliosis can develop at any location along the spine, but it most commonly develops in the thoracic spine. Knowing the precise location of the curvature is important for targeting treatment components, such as chiropractic adjustments.
Additionally, certain curvature locations correlate with specific symptoms, guiding the treatment approach. This classification helps name the condition, such as mild adolescent idiopathic thoraco-lumbar scoliosis, indicating severity, age, cause, and curvature location.

What Does Mild Scoliosis Look Like?
No two cases of scoliosis are the same. Not only does scoliosis range widely in severity from mild to moderate and severe to very severe, there are also different types of scoliosis patients can develop.
Condition type is determined by causation; the majority of known cases are idiopathic, meaning not clearly associated with a single-known cause, and the remaining condition types are associated with known causes: neuromuscular scoliosis, congenital scoliosis, and degenerative scoliosis.
In addition, there are also different curvature locations, types, and patterns that are known to cause different symptoms, affect different areas of the body, and have different treatment needs.
All of these cases of scoliosis will look different based on patient age, condition type, severity, and curvature location.
Very mild scoliosis, truthfully, is unlikely to look like anything; as in, a person with very mild scoliosis is likely to be unaware of their condition, and it’s also highly unlikely that anyone other than a professional trained in the condition’s early signs would notice it.
So a person with very mild scoliosis is likely to look the same as people without scoliosis, but it is important to understand that as a progressive condition, even scoliosis that’s diagnosed as mild can progress to become moderate, severe, or very-severe scoliosis.
What Does Mild Scoliosis Feel Like?
Scoliosis will feel different from patient to patient based on the factors mentioned above: patient age, condition type, severity, and curvature location.
When it comes to how scoliosis feels, severity is key; mild scoliosis doesn’t commonly cause functional deficits, and as scoliosis doesn’t become a compressive condition until skeletal maturity has been reached, it’s not often painful for children.
In young patients whose spines are still growing, the constant lengthening motion of a growing spine counteracts the compressive force of the unnatural spinal curve, so while pain is the main symptom of scoliosis in adults, it’s not a common symptom of childhood scoliosis.
While scoliosis affects all ages, it’s most prevalent in adolescents, and in cases of very mild adolescent idiopathic scoliosis, the size of the scoliotic curve is small, and the angle of trunk rotation (ATR) is also mild.
So while it’s possible that very mild scoliosis will also go unnoticed in adults, for adults, it’s more likely that any degree of scoliosis will cause some level of pain due to compression.
For children with very mild scoliosis, it’s likely that they will look and feel the same as their peers without the condition; it’s often not until cases of mild scoliosis progress to become moderate scoliosis that their effects become noticeable enough to lead to a diagnosis and treatment.
While there are never treatment guarantees, early detection is associated with treatment success, and the best way to minimize how scoliosis affects the spine, its surroundings, and the entire body is a proactive conservative treatment plan.
The good thing about being diagnosed with very mild scoliosis is that smaller curves are simpler to treat, so if early detection has led to a diagnosis and is responded to with immediate treatment, there are fewer limits to what can be achieved.
Mild Scoliosis and Early Detection
Two important features of scoliosis to understand is that it is both progressive and incurable.
What this means is that it’s in the condition’s nature to worsen over time and that there is no known cure.
While this can be very frightening for someone recently diagnosed to hear, I remind patients and their families that while we might not be able to cure it, we have many resources at our disposal to help us treat and manage it effectively.
While a spinal disorder marked by an abnormal bend and twist seems like it would be easy to spot, this is not always the case, especially with mild forms of the condition.
As mild scoliosis is the first stop on the condition’s progressive line, this is also the stage that carries the fewest/mildest symptoms, and those that are present are often not noticeable to anyone other than a scoliosis specialist who is trained to recognize the condition’s subtle early signs.
Postural changes that develop during this stage are subtle, and very often, the person and their families will not notice them until progression occurs and the condition moves into the next stages: moderate and severe scoliosis.
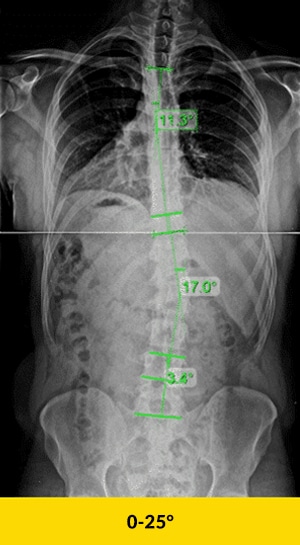
Mild scoliosis refers to a condition where the spine curves to the side, typically at an angle of less than 20 degrees. For instance, a 17-degree scoliosis curvature is considered mild. Mild scoliosis can manifest as a mild right convex scoliosis in the lumbar spine or other parts of the spine. Treatment options for mild scoliosis may include physical therapy to help manage the scoliosis curve and prevent further progression.
So for those wondering what does mild scoliosis look like? The answer is, in many cases, patients with mild scoliosis don’t look much different on the outside, at least not to those with an untrained eye.
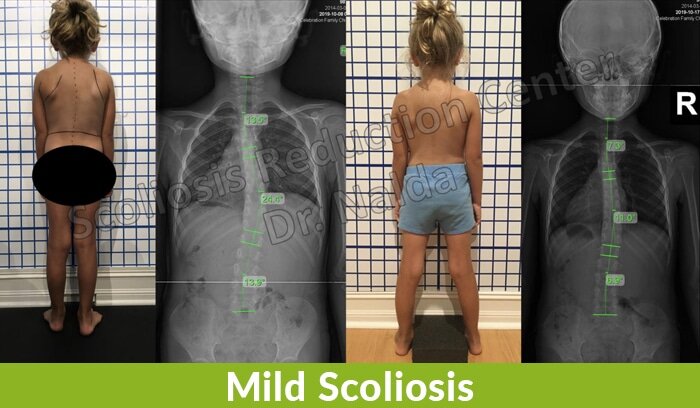
The before-and-after treatment X-ray images show what’s going on with the spine, but at this stage, these changes are rarely noticeable to the naked eye or to those with no scoliosis-specific experience.
If you suspect you have scoliosis, or suspect a loved one does, don’t hesitate to reach out to us here so we can help determine whether scoliosis is present or not.
This brings us to the next question you might be asking: what are the symptoms of mild scoliosis?
Symptoms of Mild Scoliosis
Scoliosis is a difficult condition to talk about in general terms; this is because it ranges so much in severity from mild to moderate and severe.
Even within one of those categories, such as mild scoliosis, there is a lot of variance, and no two patients will experience their condition in the exact same way, including symptoms.
That being said, especially in the context of early diagnosis, there are some common symptoms that can be watched out for.
Mild Scoliosis Pain
While most cases of adolescent idiopathic scoliosis aren’t painful, patients may still experience scoliosis-related pain as the curvature progresses. About 20 percent of adolescents report muscle pain, which can worsen over time. Adults experience scoliosis pain differently due to spinal compression, causing neck and back pain, and radiating pain into limbs from pinched nerves.
Mild scoliosis can also cause hip pain if pelvic symmetry is affected. The longer scoliosis goes untreated, the more likely it is to cause pain. If you experience scoliosis-related pain, seek help for active treatment and relief.
Uneven Posture
Uneven shoulders and hips can indicate mild scoliosis, as can any sign of body asymmetry.
Other postural changes include an uncentered head over the torso, arms appearing to hang at different lengths, one side of the ribs protruding more, the body leaning to one side, legs seeming to hang at different lengths, one hip sitting higher, one side of the waist appearing flatter or more rounded, one shoulder blade protruding more, and uneven space between the arms and torso. These subtle changes suggest the presence of scoliosis.
Clothing Fitting Unevenly
The way clothing hangs on a body can indicate asymmetries. Subtle postural changes associated with mild scoliosis can affect clothing fit. Pay attention to sleeve cuffs and their alignment on each arm, and if shirt necklines pull more to one side.
Ill-fitting clothing isn’t a definitive sign of scoliosis, but sudden changes can prompt further investigation. While not conclusive, these clothing fit issues can be a reason to explore scoliosis as a potential cause.
Headaches
While mild scoliosis doesn’t guarantee headaches, it can be a common issue for scoliosis patients. Curvature location can indicate likely symptoms, such as tension headaches associated with cervical spine curvatures.
An abnormal cervical spine can cause neck muscles to tighten, placing tension on the head and potentially causing migraines. Scoliosis-related headaches and migraines are also connected to cerebrospinal fluid (CSF) flow. CSF cushions the spinal cord and brain, delivers nutrients, and removes waste. Interruptions in CSF flow due to scoliosis can lead to debilitating headaches as CSF levels in the brain decrease.
Balance and Coordination Issues
Balance and coordination issues can be difficult to spot early, especially in adolescents. Considering adolescent slouch and reminders to “stand up straight,” changes in balance and coordination can seem like teenage awkwardness.
Testing balance by having the person close their eyes and balance on one leg for 30 seconds can help; most people can do this. For those with scoliosis, recognizing body positioning without visual cues (proprioception) is challenging. Balance and coordination issues, while subtle, can suggest mild scoliosis.
Changes in Gait
Changes in gait can reveal mild scoliosis. How a person walks can indicate their condition. Mild scoliosis may show in reduced arm swing and less counter-rotating motion of the hips and shoulders.
Asymmetrical motion during walking can also be a sign. While having one of these issues might not mean scoliosis is present, multiple postural issues can indicate the need for further testing.
Early assessment can prevent the harm of undiagnosed and unimpeded scoliosis progression.

Mild Scoliosis Progression
As previously mentioned, scoliosis is progressive, and this means that it is virtually guaranteed to get worse over time, if left untreated.
Part of the challenge of treating mild scoliosis, in addition to early detection, is that while we know the biggest trigger for progression is growth, there is no way to tell precisely at what pace a patient’s spine is going to respond to that growth.
I believe that patients have the best chance for treatment success when their condition is caught during the mild stage.
As AIS is the condition’s most common form, it’s this age group that faces the biggest risk for rapid progression.
If an adolescent’s condition was left undiagnosed and untreated until its symptoms became severe enough to reach a diagnosis in adulthood, progression tends to slow, but it is still an issue.
In most cases of adult idiopathic scoliosis, these are continuations of AIS that were not diagnosed and treated during adolescence, most often because the person was simply unaware of their condition.
By the time these adults are diagnosed, obviously their condition has been left to progress unimpeded for quite some time, and it’s not until the condition started to produce noticeable symptoms that they sought a diagnosis and treatment.
So let’s say an adult comes in to see me because of back pain, and I diagnose them with mild scoliosis with a Cobb angle measurement of 24 degrees.
Even with the slower progression characteristic of adulthood, let’s say of one degree a year, over 10 years, that adult now has a Cobb angle of 34 degrees and is that much closer to reaching that surgical threshold.
You can see how, even slow progression, has a cumulative effect that can equal up to a large abnormal spinal curvature.
My point is progression is progression; whether it happens slowly or quickly, the end result of a more severe form of the condition is virtually inevitable, if left untreated.
This moves us into the topic of treatment options for mild scoliosis, which brings us to that fork in the road that every scoliosis patient has to face: choosing a treatment approach.
Mild Scoliosis Treatment Options
As is also the case with moderate and severe scoliosis, there are two main scoliosis-treatment approaches for mild scoliosis: traditional and functional.
While the traditional approach is still a choice for many, I want people to make that choice out of knowledge and power, and to me, this means being fully aware of all treatment options available, including known benefits and risks of each.
Traditional Approach to Treating Mild Scoliosis
When it comes to the traditional approach for treating mild scoliosis, there is not a whole lot to say because this approach does nothing proactive during this early stage; instead, patients are told to watch and wait to see if/how fast their condition will progress.
For mild and moderate cases, other than monitoring, and possibly bracing, there is typically nothing done in the form of active treatment, until the patient’s degree of curvature reaches the surgical threshold.
The issue is that there is no way to know what would have happened had treatment been started earlier.
In many cases, treatment started early in the condition’s progressive line means avoiding the hardships of reaching more severe stages, especially when severe scoliosis can come with the recommendation for spinal-fusion surgery.
In the traditional approach, people watch and wait while patients’ conditions progress, which they are bound to do, and to me, this is wasting valuable treatment time.
Once a patient crosses that surgical threshold at around 45 degrees, shows continued progression, and bracing has proved ineffectual (if attempted), they are funnelled towards surgery as the best way to stop the condition from progressing further.
So to be clear, if a patient with mild scoliosis is referred to a spinal surgeon for treatment options, no proactive treatment is done during this stage; in the traditional approach, the strategy is to monitor the condition to see how the spine responds to growth (AIS) and progresses.
If mild and moderate scoliosis is left untreated, or not treated proactively, it’s virtually guaranteed to progress, and if a patient with mild scoliosis progresses into the moderate and then severe stage, surgery can be presented as a positive treatment option, and that comes with a whole lot of potential risks and side effects, not to mention the cost.
This brings us to a question most people freshly diagnosed with mild scoliosis would ask: does mild scoliosis require surgery?
Does Mild Scoliosis Require Surgery?
The question of whether mild scoliosis requires surgery has a complex answer.
In simple terms: no, mild scoliosis does not require surgery. However, if mild scoliosis is left untreated and progresses into the severe stage, for those on the traditional-treatment path, they could end up being told surgery is necessary.
In order for a person’s scoliosis to be considered in the surgical threshold, in most cases, this involves curvatures of 40+ degrees, but again, every case is different.
Spinal fusion surgery will never be necessary for treating mild scoliosis because in this stage, curvatures are far below the surgical level, and even for supporters of spinal fusion for severe scoliosis, no surgeon would perform such an invasive procedure on a patient whose curvature is not even close to that surgical level.
Spinal fusion should only be used, in my opinion, as an absolute last resort, after all other options have been explored and failed.
This is because spinal fusion is permanent. If a patient is unhappy with the results, or the procedure fails for any number of reasons, the only possible recourse is more surgery.
If a patient is unhappy with the results of our functional approach, there is no harm done. As it is a natural and noninvasive approach, there are few, if any, side effects, and nothing is irreversible.
Scoliosis surgery also comes with some heavy side effects such as reduced flexibility, and it’s not uncommon for patients to report an increase in scoliosis-related pain post surgery.
In addition, there is also no guarantee that a patient’s scoliosis won’t continue to progress, despite having undergone the invasive surgery.
To answer the question clearly, no surgeon is going to perform spinal fusion on a person with mild scoliosis because not only would it be unnecessary, it would mean exposing that patient to all the potential risks, complications, and costs associated with the surgery.
Here at the Scoliosis Reduction Center®, this is why our functional treatment approach is more proactive than reactive.
We want to reduce our patients’ abnormal curvatures while their conditions are in the mildest form possible; we strive for this to improve their overall quality of life, and a big part of that is avoiding the hardships of severe scoliosis and potentially facing spinal-fusion surgery down the road
Now, let’s explore our treatment approach for a typical case of AIS diagnosed in the mild stage.
Functional Approach to Treating Mild Scoliosis
If a patient came in to see me with scoliosis concerns, I would give them a physical exam and take their histories. If I saw some indicators, I would order a scoliosis X-ray to take actual measurements and confirm that structural scoliosis is present.
If the Cobb angle measured at more than 10 degrees, but less than 25, and included rotation, I would sit down with the patient, and their family, and give them their diagnosis of mild scoliosis.
From there, I would recommend starting treatment as soon as possible. I would explain the benefits of this in the context of progression and how if left alone, related symptoms and degree of curvature are virtually guaranteed to increase.
From the X-ray and exam, I would have all the condition information I need to design a treatment approach moving forward.
Our treatment approach would also involve a lot of monitoring to observe how growth affects the spine, but the difference between our monitoring and monitoring in the traditional approach is that we would actively respond.
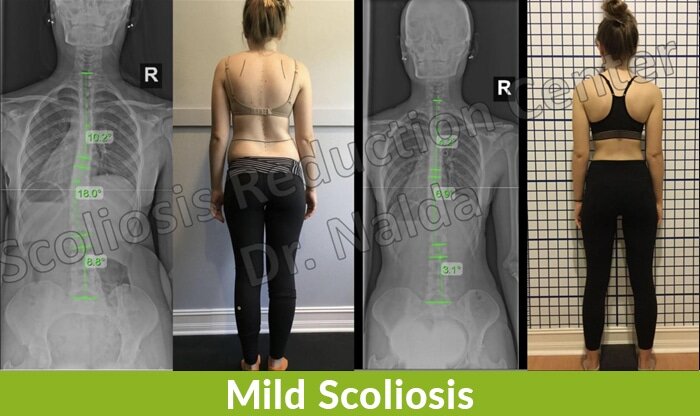
From the following X-ray images taken before and after treatment, you can see the difference that active treatment can make.
Our integrative approach combines multiple treatment disciplines. This is highly beneficial for scoliosis patients not only because they can benefit from the different merits of each approach, but because it allows us to fully customize our treatment plans to address the individual patients and their conditions.
In the mild stage, our ultimate treatment goal is to impact the condition on a structural level by reducing the curvature, lessening related symptoms, and stopping the condition from ever reaching the moderate and severe stage of progression.
Different Facets of Functional Treatment for Mild Scoliosis
As mentioned, here at the Center, we combine multiple treatment disciplines.
These disciplines are scoliosis-specific and include targeted chiropractic adjustments, active and passive rehabilitation, exercises, and corrective bracing.
We combine these disciplines based on the needs of the patient and their condition, then we adjust and apportion them differently as we observe how they are working together and how the spine is responding.
The great thing about this approach, in addition to its efficacy, is how engaged the patient is throughout the process.
Obviously, it would be hard for an adolescent patient freshly diagnosed with mild scoliosis to see themselves as fortunate, but I do my best to accentuate the positives of early detection and how it increases treatment success.
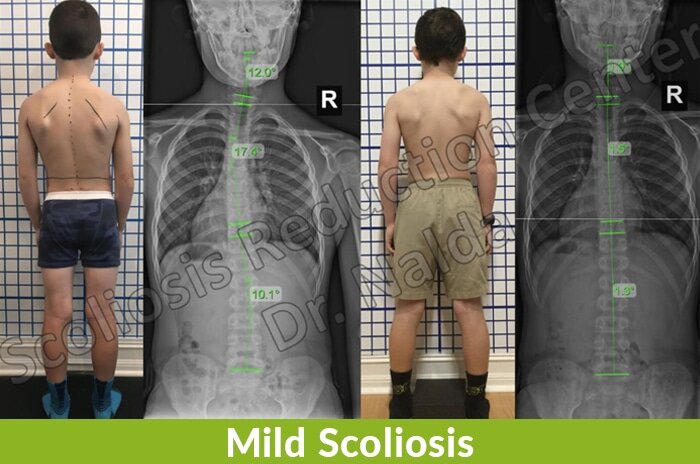
You can see, by looking at the below X-ray images taken before and after treatment, just how effective our functional approach can be; here, the patient’s curvature has been reduced and improved upon the postural asymmetries caused by the condition.
In addition, active treatment helps patients maintain feelings of power and control over their condition, bodies, and lives, and this translates into a better attitude, better treatment efficacy, and improved mental health.
Here, I would like to say a few words to clearly explain what each facet of treatment involves:
Scoliosis-specific chiropractic – for this treatment facet, we use scoliosis-specific chiropractic adjustments to try and manipulate the spine to move out of the unhealthy curvature and restore as much of the spine’s healthy curves as possible.
Traditionally, the place of chiropractic in scoliosis treatment has been questioned, but as general chiropractic will most certainly fall short when it comes to treating scoliosis, scoliosis-specific chiropractic is different and has the power to impact the condition in very positive ways.
Scoliosis-specific therapy – the goal of scoliosis-specific therapy is to passively mobilize the spine into a corrective position.
This facet of treatment would include traction, de-rotation, and vibration.
Here at the Center, we use multiple types of equipment that were designed specifically for reducing scoliosis.
Scoliosis-specific exercises (SSEs) – for a long time, it was questioned just where and if exercise fit into scoliosis treatment; we have since learned that scoliosis-specific exercises, when done correctly and customized to a patient’s condition, can be extremely effective.
These self-correction exercises are customized to each patient’s ability and curvature type/severity; they would include a combination of exercises that are movement-based, isometric, or reflexive.
SSEs are also a great tool for mild scoliosis pain management. Keeping the spine and its surrounding muscles and tendons as loose and strong as possible is a healthy and proactive way to manage and reduce scoliosis-related back and muscle pain.
Here at the Center, we have all the state-of-the-art exercise equipment needed to facilitate this component of treatment.
Corrective bracing – for those who have done their due diligence in researching scoliosis treatment, they have likely come across the reference to bracing as a component of treatment.
For those wondering why sometimes the term ‘corrective’ is applied to bracing, and sometimes not, this is because not all braces are created equal and have the same treatment goal in mind.
Corrective braces have a structural curvature reduction as its end goal, whereas common traditional braces, such as the Boston brace, have a different goal.
As mentioned earlier, bracing is the only form of active treatment that takes place in the traditional approach, prior to reaching that surgical threshold, and the most common brace used in the traditional approach is the Boston.
The Boston brace, like scoliosis surgery, doesn’t have correction as its ultimate goal, but rather slowing/stopping progression. It does this by squeezing the spine at certain points along the curvature and holding it in a corrective position, but doesn’t actually correct it.
With our functional treatment approach, we use a completely different type of brace: the 3D corrective ScoliBrace.
The big difference between the Boston brace and the ScoliBrace is in design and treatment goal. The ScoliBrace is designed to actually reduce the curvature while being worn.
In addition, it is custom manufactured based on each patient’s curvature type, body type, and level of spinal flexibility.
The difference in design is related to the contrasting end goals; instead of slowing/stopping progression as the Boston brace hopes to do, the ScoliBrace strives to actually correct the scoliosis by reducing the curvature and supporting the reduction.
So when it comes to the best mild scoliosis brace, a brace that is corrective and customized has the best shot of actually impacting the scoliosis on a structural level, which is precisely what successful treatment entails.
If you would like to learn more about our proactive functional treatment approach here at the Center, don’t hesitate to reach out.
Mild Idiopathic Scoliosis in Adults
As the condition’s most common form (AIS) accounts for 80 percent of known diagnosed cases, I have focused the article on this form of the condition.
While the majority of my patients are adolescents in the moderate stage, let’s not forget that adults can develop the condition as well. Scoliosis in adults has two main forms: idiopathic and degenerative.
When idiopathic scoliosis appears in adulthood, it is most commonly an extension of AIS.
As discussed, it’s not always easy to diagnose AIS, and it’s not uncommon for adolescents to grow and develop with their scoliosis in tow, until growth stops in adulthood, the condition becomes painful, and this is what brings them in to see me for a diagnosis.
In these cases, our treatment goal is to reduce the abnormal curvature back to where it was before it starting producing noticeable symptoms like back and muscle pain.
Mild Degenerative Scoliosis in Adults
Degenerative scoliosis most often appears after the age of 40. This develops due to the natural degenerative effects of aging on the spine, commonly affecting the intervertebral discs.
The intervertebral discs act as cushions between the individual vertebra and shock absorbers for evenly distributing the force of impact.
When the discs that sit between the vertebrae of the spine start to degrade, this can cause slippage to occur, and the spine can start to gradually bend out of alignment and develop scoliosis as a result.
In these types of cases, it’s pain and discomfort that brings adults in to see me, and once we do an X-ray, we can gauge the health of the spine, its intervertebral discs, and give the patient their diagnosis.
In women, changes to hormone levels and bone density due to menopause can also play a role.
Regardless of age or condition severity, there is a potential treatment plan for each and every patient we see.
Here at the Center, our goal is to help patients avoid reaching the higher stages of progression; the first step to reaching that end goal is connecting with patients in need.
Reach out to us here if you feel you, or a loved one, are one of these patients.
Understanding Scoliosis
What Is Scoliosis?
the spine. This condition can affect individuals of any age, but it is most commonly diagnosed during adolescence. Scoliosis can be classified into several types, including idiopathic scoliosis, congenital scoliosis, and degenerative scoliosis.
Idiopathic scoliosis is the most prevalent form, accounting for approximately 80% of all scoliosis cases. This type of scoliosis has no single known cause and is characterized by a lateral curvature of the spine, which can occur in the thoracic, lumbar, or thoracolumbar regions. Congenital scoliosis, on the other hand, is present at birth and results from malformations of the spine during fetal development. Degenerative scoliosis typically occurs in adults due to the natural aging process and the degeneration of spinal discs and joints.
Understanding the type of scoliosis is crucial for determining the most effective treatment approach and managing the condition effectively.
Scoliosis Diagnosis
Diagnosing scoliosis involves a comprehensive approach that includes a physical examination, medical history review, and imaging tests. During the physical exam, a healthcare provider will assess the shape of the spine, posture, and alignment. They will look for signs of spinal curvatures and asymmetries, such as uneven shoulders or hips.
The medical history review is equally important, as it helps the provider understand any potential genetic factors, symptoms, and lifestyle aspects that may contribute to the condition. Questions about family medical history, the onset of symptoms, and any previous treatments are typically asked.
Imaging tests, such as X-rays are essential for confirming the diagnosis and determining the degree of scoliosis. These tests provide detailed images of the spine, allowing the healthcare provider to measure the Cobb angle and assess the severity of the curvature. Accurate diagnosis is the first step in developing a personalized treatment plan that addresses the specific needs of the patient.
The Importance of Early Intervention
Early intervention is crucial in managing scoliosis effectively. For mild scoliosis patients, receiving early treatment can significantly reduce the spinal curvature and prevent further progression. Early intervention not only addresses the physical aspects of scoliosis but also helps prevent potential complications, such as respiratory and cardiovascular problems, as well as back pain.
By starting treatment early, patients can improve their overall quality of life and reduce the risk of long-term disability. Early intervention often involves a combination of physical therapy, exercises, and, in some cases, bracing. These treatments aim to strengthen the muscles supporting the spine, improve posture, and halt the progression of the spinal curvature.
The proactive approach to treating mild scoliosis underscores the importance of early detection and immediate response. By addressing the condition in its early stages, patients can avoid the more severe consequences of scoliosis and maintain a healthier, more active lifestyle.
Scoliosis’ Effect on Overall Health
Scoliosis can have a significant impact on overall health, particularly if left untreated or not treated proactively. While mild scoliosis symptoms may not always be noticeable, the condition can progress and lead to more severe symptoms over time. These symptoms can include back pain, muscle stiffness, and fatigue, which can affect daily activities and overall well-being.
In severe cases, scoliosis can cause respiratory and cardiovascular problems due to the abnormal curvature of the spine affecting the chest cavity. Additionally, patients may experience numbness, tingling, and discomfort in the arms and legs due to nerve compression.
Therefore, it is essential to seek medical attention if symptoms persist or worsen over time. Early diagnosis and treatment can help manage the condition effectively, prevent complications, and improve the patient’s quality of life. By addressing scoliosis proactively, patients can maintain better overall health and avoid the more severe consequences of the condition.
Conclusion
When it comes to mild scoliosis, this is the earliest stage of the condition.
Defined as a spinal disorder with a Cobb angle measurement between 10 and 25 degrees that coincides with rotation, mild scoliosis is the best time to start treatment.
While there are multiple benefits to starting active treatment while a patient’s scoliosis is still mild, this can be particularly challenging because early detection isn’t always possible, which is why the majority of my patients are in the moderate stage.
Mild scoliosis does have some telltale signs to look out for, but many of these are very subtle and difficult to spot.
Let’s also not forget that in AIS, there is the possibility that adolescents wouldn’t share the discovery of any bodily changes they don’t understand or feel sets them apart from their peers.
I’ve said it before, and I’ll say it again: there is no harm to reducing an already-mild curvature to even smaller, but there is most certainly harm done by simply watching while a patient’s condition progresses from mild to moderate and severe.
Here at the Scoliosis Reduction Center®, we feel privileged to walk alongside patients on their scoliosis journey.
For those I diagnose with mild scoliosis, I enjoy sharing with them, and their families, the potential positive treatment outcomes ahead.
With some hard work and patience, we can help these mild-scoliosis patients avoid the hardships of the moderate and severe stages of progression altogether.
Consultation & Information Request
If you want to schedule a consultation, or just want more information you can call 321-939-2328 or use this form. We can call or email you to discuss your options.

